The Veterans Community Care Program (VCCP)—established in response to the 2014 wait time scandals at multiple Veterans Affairs medical centers (VAMC)—allows eligible veterans to receive care from networks of approved health care providers in their local communities. To be eligible, veterans must meet certain criteria, such as living too far from a local VAMC, needing services not offered at a local facility, or a provider deciding care in the community is in the veteran’s best interest.
Since its 2018 expansion through the MISSION Act, the VCCP has seen a steady increase in the number of enrollees. The rising use of the VCCP, however, has paralleled a rise in expenditures diverted to pay for care received in the community, up from $7.9 billion in 2014 to $18.5 billion in 2021. This sum represents approximately 44 percent of the Veterans Health Administration’s (VHA) health care services expenditures across all settings. Understandably, this has rung some alarm bells, with critics arguing that increasing VCCP costs will make sustaining the VA’s existing healthcare infrastructure impossible. However, there is reason to believe that the VCCP is not the sole driver of rising costs in the VA.
Cost of the VCCP
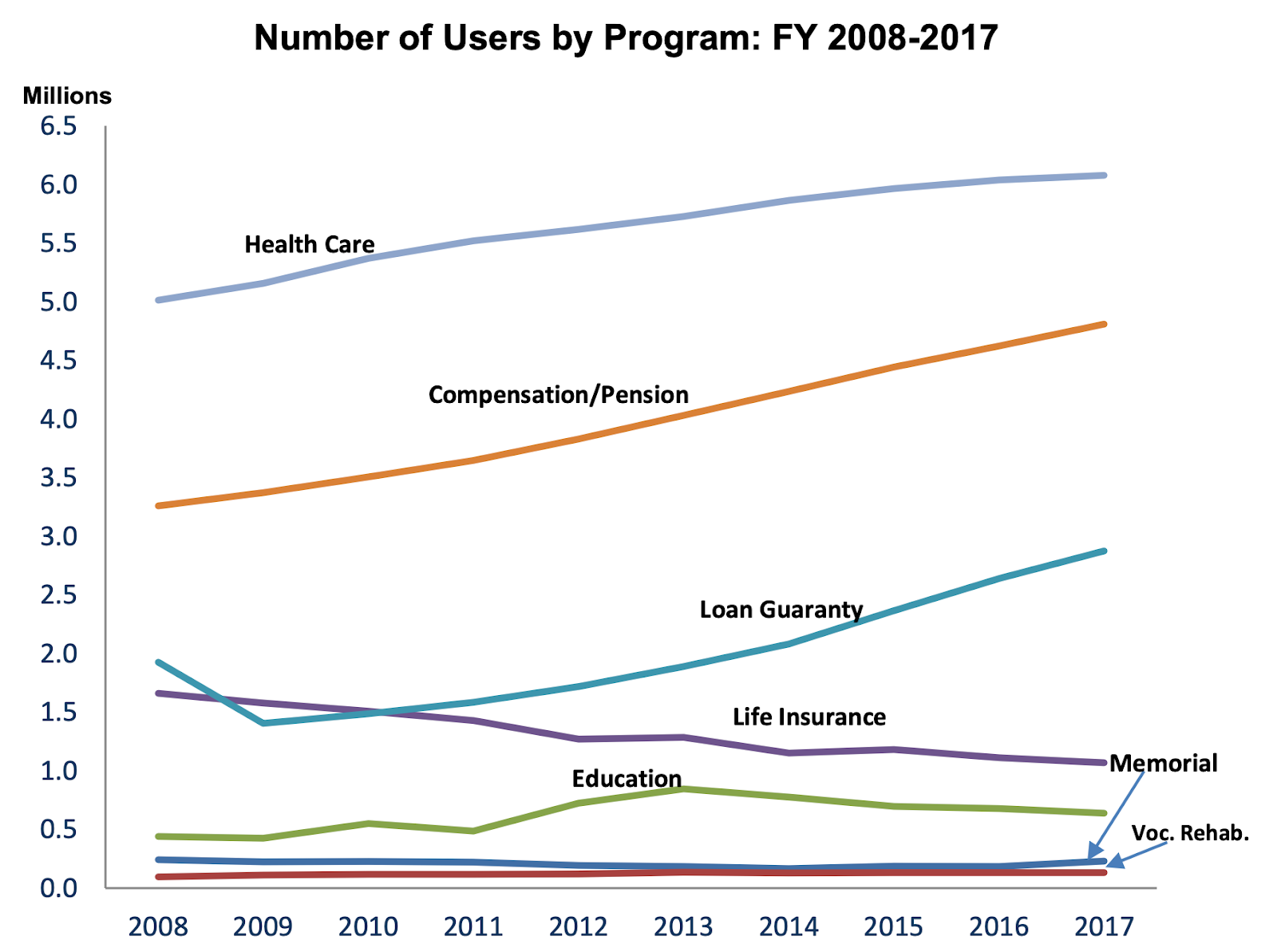
Understandably, some are worried about the VCCP's sustainability. As shown below, rising costs parallel the increases in eligibility for the VCCP, increasing as more veterans become eligible to receive care in the community. Thus, the most natural explanation for the rise in cost is that it is a direct result of the VA having to pay for more care through the VCCP. If the VA is paying for more care in the VCCP, then they should ideally be paying for less care at VAMCs, thus balancing out the total costs. In reality, this is not happening, primarily for two reasons. First, the VA maintains many high-cost facilities that should be shut down. Second, the VA is experiencing increases in healthcare utilization by veterans at VAMCs despite a 14 percent decline in the number of veterans since 2008.
Figure 1. Trends in utilization of VA benefits by veterans, 2008–2017.
Compared to the cost of care per beneficiary in the VA, the estimated cost of care in the VCCP is substantially lower. On average, the VHA spent $14,750 per veteran patient in 2021—which, for reference, is remarkably close to the estimated $14,348 spent per beneficiary in Medicare. However, based on data published by the Congressional Budget Office, the annual expenditures for veterans enrolled in the VCCP has only grown from $6,076 per veteran in 2014 to $7,347 per veteran in 2020.
Notably, the VHA cost per veteran includes expenditures on the VCCP. However, only about 25 percent of veterans enrolled in the VA are currently eligible for care in the VCCP. Thus, even after accounting for expenditures on the VCCP, the cost is still estimated at over $12,000 per veteran for care received in the VHA, which exceeds the cost of care in the VCCP by a substantial margin.
With costs being substantially less in the VCCP, it is reasonable to wonder whether the quality of care lags behind the VA. Of the scant available data comparing the VCCP to the VA, quality appears to be roughly equivalent. For example, one study examining elective knee replacements found that while the VA had fewer complication rates than the VCCP, comparisons between entire VA facilities showed comparable levels of quality to their VCCP counterparts.
Although healthcare in the VCCP is cheaper per capita than the VA, one reason to worry about the amount of money flowing to the VCCP is that the VA failed to cut costs when their patient population shifted. The VA has 1,240 facilities throughout the United States, 336 of which are currently vacant or less than 50 percent occupied. Making matters worse, approximately 70 percent of VA facilities were built over 50 years ago, whereas private hospitals average an age of 8.5 years. Annual maintenance cost estimates exceed $1 billion now, and projected capital needs over the next 10 years may be over $60 billion. As previously discussed at length in our plan to achieve healthcare independence for veterans, selling, repurposing, or leasing unused or inhabitable facilities is a workable solution to rein in VA's costs.
In addition to the VCCP being cheaper per capita than care provided in the VA, it will also benefit lower-income veterans. Most veterans have ancillary insurance, either through Medicare, Medicaid, or private insurance. Conversely, about one in five veterans have no additional public or private coverage aside from the VA, and lack of additional insurance coverage is highest among veterans with an income less than $35,000 per year. For lower income veterans who have trouble accessing the VA system - one of the very criteria used to qualify for the VCCP - the VCCP may serve as a critical lifeline to care.
The VCCP is worth the cost
Caring for veterans in the VCCP is cheaper on a per-patient basis than it is in the VA and rising VA costs are not the result of the VCCP. Even when accounting for veterans who receive care in both the VA and VCCP, the VCCP provides cheaper healthcare per capita. Aside from the price tag, increasing enrollment in the VCCP speaks for itself: veterans want community care. The VA should give it to them.


